Patellofemoral Pain
Patellofemoral Pain
What is the patellofemoral joint (PFJ)?
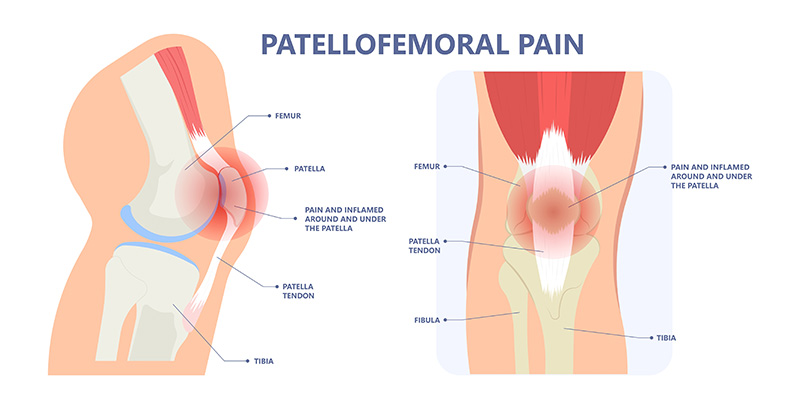
The patellofemoral joint (PFJ) is at the front of the knee and is formed between the meeting of the back of the patella (kneecap) and the trochlea (front of the femur). It is a very important part of the knee for good function and a complex area.
Overall, it is probably responsible for more consultations than any other part of the knee. Pain and symptoms from this region over the front of the knee are extremely common and a frequent knee complaint. It is often simply referred to as “anterior knee pain”.
Presentation
Pain can be generated from numerous structures:
- articular joint surface cartilage
- the bone
- tendons
- muscles
- the fat pad
- superficial bursal tissues.
It may be secondary to an injury or be more gradual and prolonged in onset. It typically causes pain when the knee is loaded in a flexion position such as squatting, getting out of low seated positions, the use of stairs (especially descent) and walking on inclines.
Pain from this area can affect all ages from teens to the elderly. For some, pain is present only in demanding activity and for others it is in simpler day to day tasks.
Diagnosis
X-Rays and MRI scans can be a useful addition to identify the likely source of pain and help plan the most appropriate treatment and rehabilitation.
Initial Treatment
The mainstay and initial treatment of nearly all patellofemoral pain issues will be non-operative. There is often no quick fix therefore patience and hard work with a good physiotherapist is generally the way forward. The key is to start appropriate strengthening programmes and to ensure adequate control when loading their joints in activities. A lot can be achieved in addressing these deficits and it means working on global leg strength, improving the gluteal muscles (hip) and core (trunk) muscles in particular.easier.
Prognosis
Fortunately, most individuals can be managed successfully with a combination of:
- activity modification
- education
- managing expectations and loads
- strengthening programmes
- improving biomechanics
- analgesia and anti-inflammatories
- occasional injections.
The need for surgery is individualised and generally is not required unless for a very specific indication.